A 60 YRS OLD MALE WITH SOB,PEDAL EDEMA,ANURIA AND CONSTIPATION SINCE 4 DAYS(28/4/23)
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
B.Pavithra(intern)
Roll no:9
Presenting complaints:
1.Anuria since 4 days
2.SOB since 3 days
3.constipation since 2 days
4.pedal edema since 2 days.
HOPI:
Patient was apparently asymptomatic 20 yrs ago and then he was diagnosed with hypertension and on medication since then.
- He now suddenly developed anuria since 4 days,which is sudden in onset,and he is not able to feel full bladder and associated with abdominal distension.
-Sob(grade 4) since 3 days which is insidious in onset,continous relieved on lying down not associated with fever,cough and cold.
Constipation since 2 days,insidious in onset, passing flatus.
-Bilateral Pedal edema since 2 days insidious in onset,gradually progressive, pitting type upto the ankles.
H/o abdominal pain since 4 days dull aching type of pain around the umblicus.
No H/o cold,cough,fever,nausea and vomiting.
No H/o pnd,orthopnea,palpitations, chest pain or chest discomfort.
No H/o burning micturition,hematuria,nocturina and terminal dribbling of urine(before)
No h/o recent use of NSAIDS.
PAST HISTORY:
k/c/o hypertension since 20 yrs on atenolol since then
K/c/o CVA 10yrs ago left hemiparesis.
N/k/c/o Dm,tb,epilepsy,cad and thyroid disorders.
FAMILY HISTORY: Not significant.
DRUG HISTORY:
On prednisilone 5mg since 21 yrs for itching all over the body except the face.
GENERAL EXAMINATION:
Patient is conscious, coherant,cooperative.
No signs of pallor,icterus,cyanosis,clubbing and generalised lymphadenopathy.
Bilateral pedal edema present since 4 days upto ankles.
VITALS:
BP:130/80
PR:89bpm
RR:22cpm
SPO2:97@RA
TEMP:98.4F
GRBS:114 mg/dl
SYSTEMIC EXAMINATION:
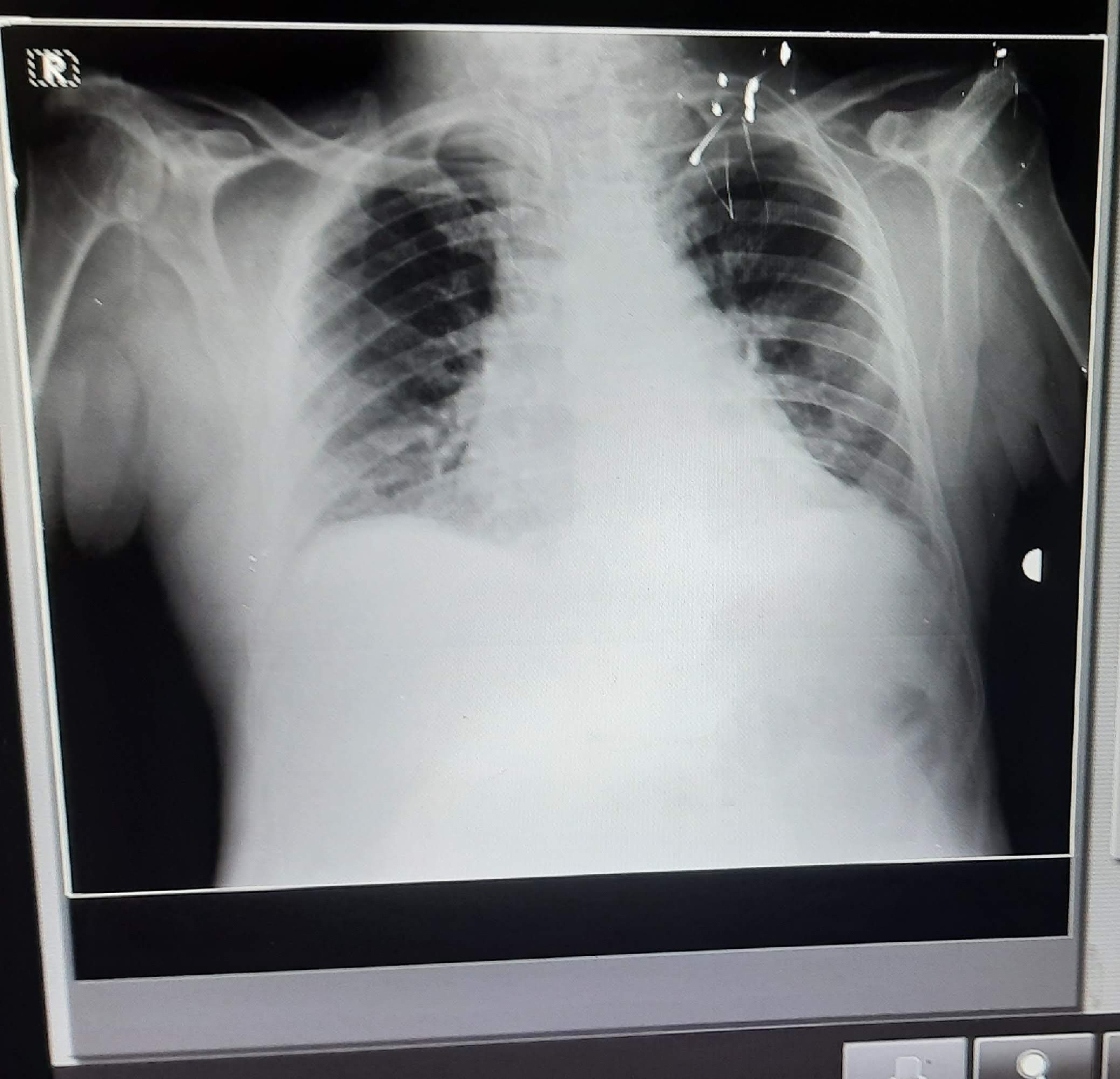
RESPIRATORY SYSTEM:
Inspection:
Chest is elliptical & bilaterally symmetrical
Trachea appears to be central.
Movements appear to be equal on both sides
No scars, sinuses, or visible pulsations
Apex impulse is not visible
Palpation:
No local rise of temperature
No tenderness
All inspection findings are confirmed: Trachea is central, movements equal on both sides
Chest expansion: symmetrical on both sides
Apex beat felt in 6th intercostal space,1 cm lateral to the midclavicular line
Tactile vocal fremitus: equal on both sides in all areas
Percussion:
Resonant note were heard in all areas
Auscultation:
Bilateral air entry present
Normal vesicular breath sounds were heard
Fine crepts heard bilaterally in infra axillary & inframammary areas.
CARDIOVASCULAR SYSTEM:
Inspection:
Chest is bilaterally symmetrical
No precordial bulge
No visible pulsations, sinus, scars, or dilated veins.
Palpation:
All inspection findings are confirmed
Apex impulse - felt in 6th intercostal space,1 cm lateral to the midclavicular line
Auscultation:
S1 s2 heard ,no murmurs
PER ABDOMEN:
Obese abdomen
Midline inverted umbilicus
No visible pulsations/engorged veins/scars/sinuses
Soft, with suprapubic tenderness, no organomegaly, no free fluid
Bowel sounds present
CENTRAL NERVOUS SYSTEM:
HMF - Intact R. L.
MOTOR SYSTEM: Power: UL 4/5 4/5
LL 0/5 0/5
TONE - Normal in right UL and LL
No tone in left UL and LL
REFLEXES - B. T. S. K. A. P.
R. +2 +2. +1. +2. --. Flexion.
L. 0 0 0 0 0 0
CRANIAL NERVES - Normal.
INVESTIGATIONS:
ECG:
2D ECHO:
USG ABDOMEN:
SEROLOGY:
HEMOGRAM:
CUE:
RFT:
SERUM IRON:





Comments
Post a Comment