A 42 years old female with SOB on exertion and generalised weakness.
This is an online E log to discuss our patients de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based inputs.
This E log book also reflects my patients-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE:
A 42 yrs old female resident of chityal,hotel worker by occupation came with the cheif complaints of SOB on exertion and generalised weakness since 1 month.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 1 month back and then she noticed SOB on exertion(while doing work) since 1 month and stopped her work 20 days back,ggeneralised weakness since 1 month.
No h/o fever,cough ,PND, orthopnea and wheez.
SEQUENCE OF EVENTS:
5 years back(in 2017) patient had chest pain and SOB on exertion and was diagnosed with anemia and had PRBC transfusion.she used to take oral iron(orofer) for 1 yr after that.
In 2021,August she came with complaints of headache(right occipital region),vomitings and giddiness and was on conservative treatment.she had one more PRBC transfusion in nalgonda gov. hospital as she couldn't afford money for blood transfusion here.
Now,she complaints of left ear pain and left ear discharge since 1 month and diagnosed with otomycosis,is on medication(candid drops)
DAILY ROUTINE:
She used to wake up in the morning at around 5 AM.she used to do all her household work and gets fresh up.she used to cook food for her daughter and sends her to the school.she has a cup of tea with biscuits and goes to work at 7 AM(hotel worker-floor cleaning,table cleaning and cleaning utensils in hotel).she has her breakfast at 11 AM in the hotel itself and continues her work.she has her lunch at 3 PM again in hotel.she returns home in the evening at around 6 PM and cooks food at home for dinner.she has her dinner at 8-9 PM and goes to bed at 10 PM.
PAST HISTORY:
No h/o diabetes,HTN,asthma,epilepsy.thyroid abnormalites and previous h/o surgeries.H/o of blood transfusion 2 times.
PERSONAL HISTORY:
Diet:vegeterian (also eats egg)
apetite:nornmal
bowel and bladder:regular
sleep:adequate
addictions:no addictions.
FAMILY HISTORY: No H/o similar complaints in the family.
MENSTRUAL HISTORY:
Regular menses-3 days, no clots , normal flow.
GENERAL EXAMINATION:
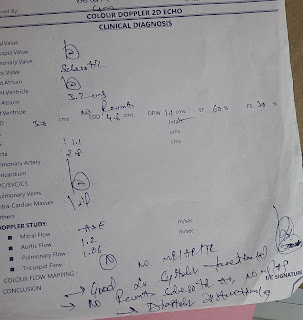
PROVISIONAL DIAGNOSIS:
microcytic hypochromic anemia(IDA?)










@Vinay 2020 KIMS PG Med @Pavan 2021 PG Kims Med Please ask this student to remove the patient identifiers visible in the ultrasound and Echo reports and also to crop the eyes and only show the palpebral conjunctiva 👺
ReplyDeleteI've cropped it and referenced it here 👉https://medicinedepartment.blogspot.com/2022/07/draft-thesis-project-plan-clinical.html?m=1
But please ask this student to correct the above asap